Deep Vein Thrombosis
What is Deep Vein Thrombosis, or ‘DVT’?
Deep Vein Thrombosis (DVT), otherwise known as deep venous thrombosis, is a blood clot in the deep veins of the body. Unlike superficial veins, deep veins cannot be seen from the skin’s surface. Thrombosis can take place in any of the veins of the body but is most frequent in the legs.
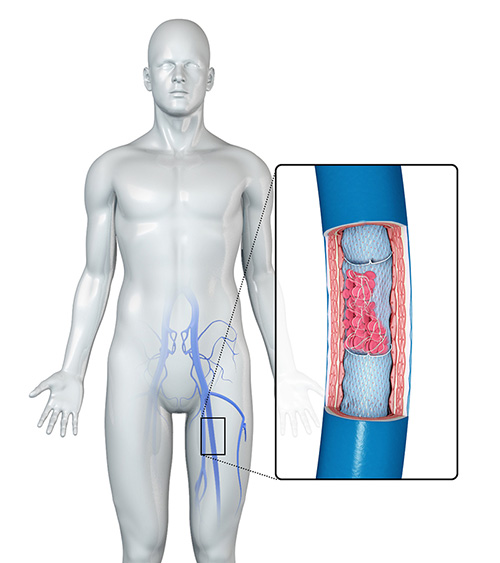
DVT in the legs can be divided into 3 main types, classified by their location:
- Ilio-femoral DVT affects the major vein in the pelvis (iliac vein) and may also involve the femoral vein in the thigh. Ilio-femoral DVT presents with the most severe symptoms and has the highest risk of subsequent complications.
- Femoro-popliteal vein DVT predominantly affects the femoral vein in the thigh and the popliteal vein behind the knee.
- Calf vein (tibial vein) DVT predominantly affects the smaller deep veins in the lower leg. Calf vein DVTs have the lowest risk of complications.
A DVT may affect all of these veins, or segments of these different veins. The 3 classfications are useful in determining severity of the DVT.
What causes Deep Vein Thrombosis?
Lowered mobility or movement in the legs, sometimes combined with an existing venous condition or weakness, is the main cause of DVT. Events such as the following can contribute to the formation of a DVT:
- Air travel - the risks of developing DVT increase as the duration of the flight increases.
- Travel, or work, in seats with minimal, cramped leg room.
- Major surgery.
- Major orthopedic surgery.
- Long periods of immobility, such as long car trips or train journey.
- Severe illness that requires a long term hospital or home bed rest.
Additionally, important risk factors for DVT are:
- Being over 40 years old
- Pregnancy
- The presence of cancer
- Hormone therapy (hormone replacement therapy or the oral contraceptive pill)
- Dehydration
- Thrombophilias (blood disorders that make clotting more likely)
- May-Thurner syndrome - a poorly recognised cause of left-sided ilio-femoral DVT
For more information on these causes and risk factors, in particular, a major cause of DVT - ‘Economy Class Syndrome’- please visit this link.
What are the signs/symptoms of Deep Vein Thrombosis?
Many patients may have minimal or no symptoms and this is known as a ‘silent DVT’, making it difficult for the patients to know that they have had, or have, a DVT.
When symptomatic, a DVT will present with:
- Pain and swelling in the affected leg, particularly in the calf.
- Skin on the calf may be slightly red and tender.
These symptoms can vary widely in their severity and are also not very specific. Many other unrelated disorders can also cause similar symptoms, so it is difficult to diagnose DVT from the above symptoms alone. Three out of four mobile patients who present with the symptoms above, do not have a DVT.
How will Deep Vein Thrombosis affect my health?
It is important to note that a DVT is most commonly caused by another existing vascular condition, or conditions, and is then exacerbated by events such as air travel, immobility, surgery or prolonged bed rest. It is likely that this existing vascular condition will also affect your health and, if left undiagnosed, may cause future recurrences of DVT, as well as other symptoms and disease that can affect quality of life. It is important to fully examine the vascular system upon the discovery of a DVT, so any and all other conditions present can be treated systematically.
In many patients, the blood clot is reabsorbed by the body, but the valves in the veins remain damaged. This damage leads to the pooling of blood and high venous pressures, causing conditions such as chronic venous insufficiency, varicose veins, or chronic ulcers. This condition is called post-thrombotic syndrome or post-phlebitic limb. These conditions predispose you to an increased risk of future DVTs.
In instances where the clot is not reabsorbed, there is a risk that the blood clot can break free and travel to the heart and brain. This can lead to stroke, heart attack or an embolism in the lung (pulmonary embolism).
Occasionally DVT can be very severe and affect the deep and superficial veins. The clot can be severe enough to critically impair the drainage and flow of blood, which can cause venous gangrene. This potentially-life threatening condition commonly has an underlying cause of cancer or a clotting disorder.
What are the stages of Deep Vein Thrombosis?
- A combination of weak walls of the veins, damaged valves in the veins, poor muscle tone in the muscles that pump the blood upwards, combined with prolonged immobility, causes the pooling of blood in the veins of the leg(s).
- The clot develops, most commonly in the calf or thigh.
- If symptomatic, the leg may swell, and the skin will redden. It may be painful.
- Examination confirms a DVT and/or underlying cause. Treatment begins immediately - see below
- Monitoring blood clot reabsorption or movement.
- If required, further treatment, such as surgery, to remove or filter the blood clot.
- A management plan is created, commonly including thinning medication and the consistent use of compression stockings.
- Concurrent treatment, surgery or repair of the venous damage or underlying conditions.
- There is a possibility that you must stay on the blood thinning medication for the rest of your life.
- Regular vascular health checks to monitor the healing and strengthening of the veins.
I think I have Deep Vein Thrombosis – What should I do?
Often you may not feel any symptoms of a DVT so you won’t know if you have one. Fortunately, if you are in certain risk groups, or have experienced events that commonly cause DVT (such as surgery or air travel), you can be proactive in understanding of the state of your venous health, and your risk of developing a DVT, through regular checkups with your GP and vascular surgeon.
If you are experiencing localised symptoms of a DVT (swelling in one or both legs, redness, and possibly, pain), visit the emergency department immediately. Provide any information that may help diagnose a DVT, such as recent flights, long journeys, immobility, surgery, use of hormones and medications, having a sedentary lifestyle, or other related vascular conditions.
It is necessary to visit the emergency department immediately if you are experiencing chest pain, particularly when taking a deep breath in, shortness of breath, unexplained cough (sometimes coughing up of blood), unexplained heart racing or pounding, passing out / losing consciousness, pain in your arms or a loss of bodily control. These severe symptoms could be indicative of a life-threatening stroke, heart attack or pulmonary embolism.
What if I don’t have my Deep Vein Thrombosis treated?
Thrombosis is important to recognise, and treat, because it may be dangerous in two ways:
Blood clot breakage: If a piece of blood clot breaks off from the veins in the legs and travels along the veins to the lungs, it can be fatal in a small number of people, and if not fatal, can make some people seriously ill.
Valve damage and subsequent vascular illness: The buildup of a clot can be both caused by vein damage, and cause further vein damage. This may cause significant problems in the legs in the future. Treatment is important to correct abnormal blood flow in the veins to prevent more serious or widespread vascular disease.
The risk of worsening vascular damage is higher for patients that are overweight, have previous thromboses, or are older women.
If you do not treat your DVT and underlying causes for the formation of the DVT, the risks of developing life-threatening conditions such as stroke, heart attack, pulmonary embolism or venous gangrene are higher. Additionally, a DVT can exacerbate related vascular conditions, causing mild to severe symptoms in the future.
What treatment options does SVS offer for Deep Vein Thrombosis?
Sydney Vascular Surgery provides a range of treatments for DVT and related conditions.
Conservative management and surveillance
Fortunately, a DVT can be treated and the risk of immediate serious complications can be reduced. The main treatment is intravenous anticoagulation and subsequent prescription for tablet anticoagulants and the regular wearing of compression stockings.
Anticoagulation means ‘anti-clotting’. Initially, an injectable anticoagulant such as Heparin will be injected daily for 5-10 days. Heparin is a fast-acting and common anticoagulation treatment. Heparin is used initially to quickly reduce the risk of further problems.
While still having Heparin, a further treatment with Warfarin is started. Warfarin is a blood thinner too, but in tablet form. Warfarin is continued for 3-6 months and requires a regular blood clotting tests to check for its effectiveness. If you have had more than one DVT, it may be important to remain on Warfarin for the rest of your life.
Compression stockings are stockings with graduations in the elasticity (compression) as they go up the leg. When worn regularly, they provide symptomatic relief of swelling and discomfort and also, importantly, increase blood flow in the veins. They come in thigh length and calf length.
SVS can also treat DVT surgically, with the following procedures:
Filter Insertion
For some patients, an anticoagulant medication treatment is dangerous, or fails to prevent a pulmonary embolism. For these patients, filter insertion is an alternative treatment specifically used to avoid a pulmonary embolism. Filter insertion involves the insertion of a small metallic sieve into the vena cava (the major vein in the leg and torso) to stop the blood clot from reaching the lung.
Thrombolysis
This is a treatment for major DVTs. Thrombolysis uses enzymes to actively dissolve the DVT, with the aim of quickly dissolving the clot to halt the symptoms and the complications of a large DVT. The enzymes are introduced into the vein, close to the DVT, via a catheter. Thrombolysis carries a risk of bleeding in other organs such as the brain, although this occurs in only a small number of patients.
Venous surgery
Surgeries such as Thermal Ablation, Phlebectomy, Vein Stripping or VenaSeal are used infrequently, but can be effective in the treatment of large DVTs where the limb may be at risk. Venous surgery must be paired with conservative management and surveillance - consider it the start of a long-term venous health plan.
Helpful Links
http://www.anzsvs.org.au/patient-information/deep-venous-thrombosis/
http://www.anzsvs.org.au/patient-information/chronic-venous-insufficiency-and-leg-ulcers/?sstat=553